 Treatment
Treatment
Your urologist and radiation oncologist will advise you on the best treatment after considering your age, general health, and the stage and grade of the prostate cancer. The side effects you are prepared to accept are also important. Your doctor may recommend active surveillance, which means you don’t have immediate treatment, but your cancer is actively monitored. If you have treatment, you may be offered one type of treatment or a combination. Surgery, radiotherapy or hormone therapy may be used.
Active surveillance
Active surveillance is when your doctor recommends no treatment or deferred (postponed) treatment but will closely monitor the cancer with regular checkups. This is sometimes called watchful waiting. While there is no standard protocol for active surveillance, it generally involves:
- frequent PSA testing, every 3–6 months
- digital rectal examinations (DREs)
- repeat biopsies to monitor cancer growth.
Having no immediate treatment may be an option if the cancer is small (low volume) and slow growing (low grade). Active surveillance may be suggested for men over 50 years old, or men who could have treatment but wish to avoid the side effects. It may be a good option if the possible treatment side effects would have more impact on your life than the cancer itself. You can always change your mind and have treatment later. If the cancer starts to grow, treatment is usually still possible with a good cure rate. Living with an untreated cancer may make you feel anxious. You may find it helpful to talk to your urologist or radiation oncologist, or you can contact the hospital social worker.
Surgery
Your doctor may suggest surgery if you have early prostate cancer, are fit for surgery and expect to live longer than 10 years. There are different types of surgery for prostate cancer.
Radical prostatectomy
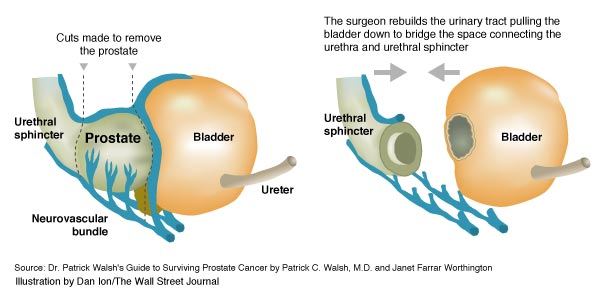
A radical prostatectomy is the removal of the entire prostate gland, part of the urethra, and the seminal vesicles, which are nearby glands that store semen. See the area enclosed by the dotted line in the diagram opposite. This surgery is usually done through a 10–12 cm cut in your lower abdomen. After the prostate is removed, the urethra is rejoined to the bladder. You will need to stay in hospital for 3–7 days to recover. A thin tube (catheter) will be used to collect your urine in a bag and you may need a catheter for 6–14 days after the surgery.
You may have some side effects from the surgery. Depending on your work and lifestyle, you should be able to return to normal activities within 4–6 weeks. Most men can resume driving within a couple of weeks, but should avoid heavy lifting for six weeks.
Nerve-sparing surgery
Nerve-sparing surgery involves the removal of the prostate and the preservation of the nerves controlling erections. These nerves can only be saved if the cancer has not spread along them and there were no problems with the nerves prior to surgery. This surgery works best with men who had good quality erections before the operation. Problems with erections are common after nerve-sparing surgery, but there are ways to manage them.
Keyhole surgery
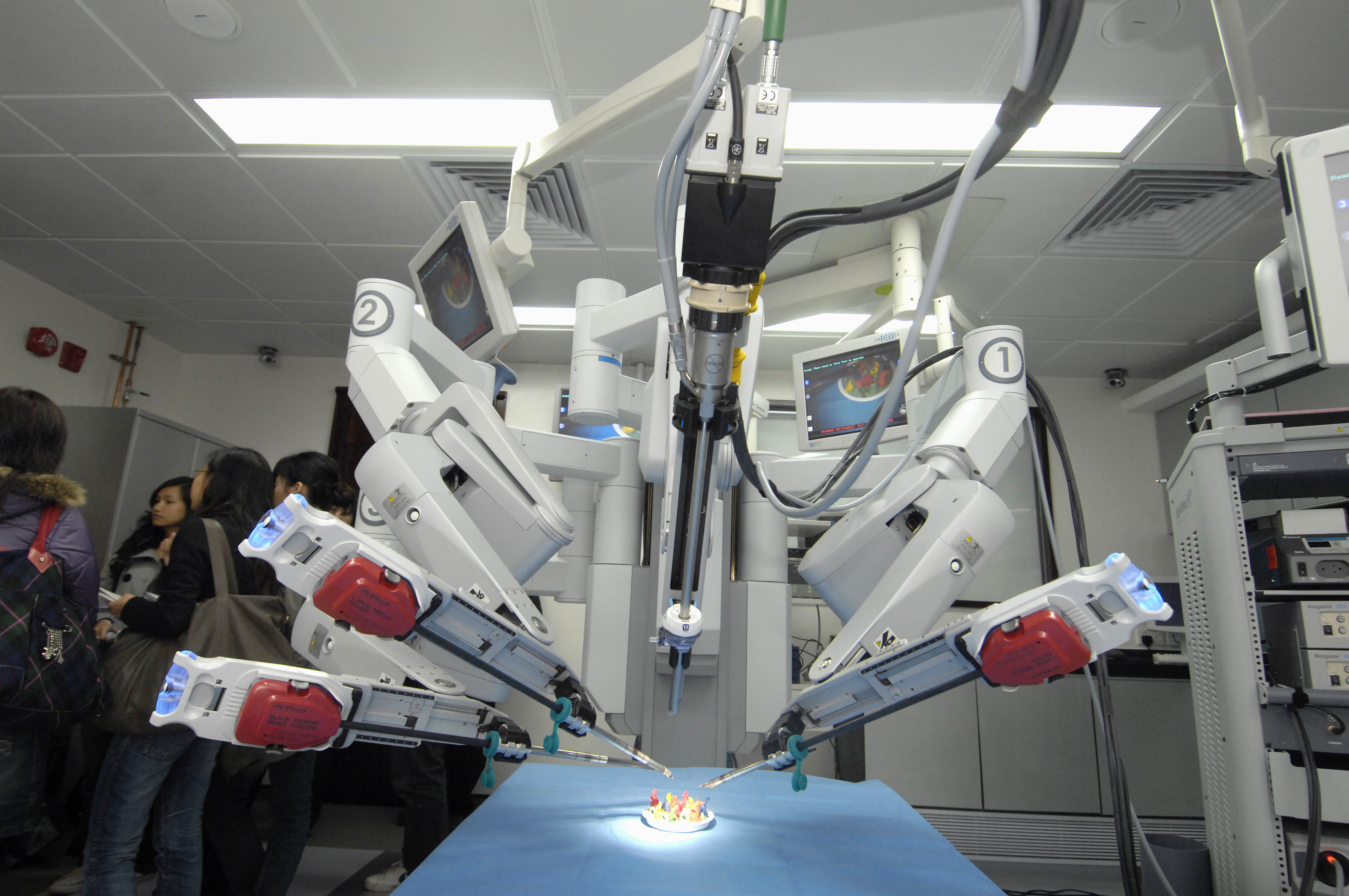
Some patients may be able to have the prostate removed via keyhole surgery. This is called a laparoscopic prostatectomy or a robot assisted laparoscopic prostatectomy. In this procedure, several small cuts are made in the skin and a small tube is passed into the abdomen. A small telescope with a camera attached (the laparoscope) is passed through the tube to allow the surgeon to see inside the abdomen. The prostate is cut away and removed through the tube.
Men who have keyhole surgery instead of open surgery have a smaller scar, faster healing and a shorter hospital stay. They usually return to normal activities within 2–3 weeks. However, there is currently no long-term evidence to show if keyhole surgery leads to fewer side effects than conventional prostatectomy. See below for information about possible side effects. Keyhole surgery is not suitable for all men. As with other types of surgery, the surgeon needs to be experienced. Also, robot-assisted surgery is more expensive than conventional prostatectomy. It is becoming more widely available as expertise is developed.
Side effects of surgery
Surgery may cause some or all of the following side effects:
- Bladder control
A radical prostatectomy may cause you to have difficulty controlling your bladder. Known as urinary incontinence, this condition usually improves within a year of the surgery. Advances in surgical techniques have made major urine control problems uncommon. There are aids and exercises for this problem and it may be helpful to see a physiotherapist as soon as possible after your operation.
If you have cloudy urine or notice any other changes when passing urine, speak to your doctor. You may have a urinary infection.
- Nerve damage
The nerves and muscles needed for erections and bladder control are near the prostate. They can be damaged during surgery, causing problems.
- Erectile dysfunction
Most men experience impotence (erection problems) after surgery. Recovery of erections can take a few years.
- Infertility
As the tubes from the testicles (vas deferens) are sealed and the prostate and seminal vesicles are removed, semen is no longer ejaculated during orgasm. This results in infertility. If you wish to have children, speak to your doctor before treatment about sperm banking or other options.